Did you know that there is a diagnosis code for virtually every part of your body plus the word “pain.”
Low back pain M54.5
Pain in the Thoracic Spine M54.6
Pain in the left foot M76.672
Chronic Bladder Pain R39.82
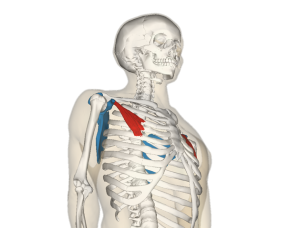
There are also diagnosis codes for significantly more detailed problems. This is often the reason for the “pain” diagnosis. I can diagnose right facet joint arthritis, or cervical degeneration that causes radiculopathy. There is value in both forms of diagnosis.
When you, the patient, comes in, you usually tell me about how you’re feeling. This discussion revolves, most commonly, around your pain. I will dig around and ask some questions and let you tell me your story. At this point, I can easily diagnose you with your specific pain diagnosis. You come in with neck pain, and I can diagnose neck pain in about 3 minutes of meeting you.
In the next step, I get to dig around and find out if there is an even more specific diagnosis that explains the “pain” diagnosis. This is the part where I rule out the really serious diagnoses, like a broken bone or a torn ligament. It is the part that takes a lot longer, occasionally more than one visit sort of longer. This is the part where we will usually throw out the fancy words. “Hip Impingement” or “Arthritis.” (And occasionally these fancy words come with an even fancier test.)
Now here is the really tricky part. Getting rid of pain can be really easy. (Tylenol, Gabapentin, Codeine) But getting rid of the fancier word part, the actual cause… now that is a lot harder. Just like diagnosing it requires a deeper understanding by your doctor to name it, it also requires a deeper understanding by you, for you to heal it.
Notice I said “You” to heal it. I can help you get rid of the pain and understand what needs to be done to heal, but the longer term changes, that is going to take more than just coming to see me a few times and taking tylenol for a couple weeks. There is a good chance you’ll need to support your body with movement, nutrition, rest and time.
This is a process. I hope to teach you everything you need to learn to heal, but it takes time. It takes time for us to peel away the layers that got you into pain in the first place and it takes time to explain each new healing step as we reach it. It will take time for you to make the changes you need to stay out of pain.
As Always,
Keep Moving.
Dr Cate


![By Anatomography (en:Anatomography (setting page of this image)) [CC BY-SA 2.1 jp (http://creativecommons.org/licenses/by-sa/2.1/jp/deed.en)], via Wikimedia Commons](http://upload.wikimedia.org/wikipedia/commons/3/31/Serratus_anterior_muscle_animation_small.gif)



